Overview
A radiofrequency ablation is a minimally invasive procedure that destroys the nerve fibers carrying pain signals to the brain. It can provide lasting relief for people with chronic pain, especially in the lower back, neck and arthritic joints. If you suffer recurrent pain and you’ve experienced good relief with a nerve block injection, you may be a candidate for a radiofrequency ablation.
What is radiofrequency ablation?
Radiofrequency ablation, also called rhizotomy, is a nonsurgical, minimally invasive procedure that uses heat to reduce or stop the transmission of pain. Radiofrequency waves ablate, or “burn,” the nerve that is causing the pain, essentially eliminating the transmission of pain signals to the brain.
This procedure is most commonly used to treat chronic pain and conditions such as arthritis of the spine (spondylosis) and sacroilitis. It is also used to treat neck, back, knee, pelvic and peripheral nerve pain. The benefits of radiofrequency ablation include: avoiding surgery, immediate pain relief, little to no recovery time, decreased need for pain medication, improved function, and a quicker return to work and other activities.
Who is a candidate?
Radiofrequency ablation is a treatment option for patients who have experienced successful pain relief after a diagnostic nerve/pain receptor block injection.
Radiofrequency ablation is done using fluoroscopic (x-ray) guidance and should NOT be performed on people who have an infection, are pregnant, or have bleeding problems.
Who performs the procedure?
The types of physicians who perform radiofrequency ablation include physiatrists (PM&R), radiologists, anesthesiologists, neurologists, and surgeons.
What happens before treatment?
The doctor who will perform the procedure reviews your medical history and previous imaging studies to plan the best location for the ablation. Be prepared to ask any questions you may have at this appointment.
Patients who are take aspirin or a blood thinning medication may need to stop taking it several days before the procedure. Discuss any medications with your doctors, including the one who prescribed the medication and the doctor who will perform the injection.
The procedure is usually performed in an outpatient special procedure suite that has access to fluoroscopy. Make arrangements to have someone drive you to and from the office or outpatient center the day of the ablation.
What happens during treatment?
At the time of the procedure, you will be asked to sign consent forms, list medications you are presently taking, and if you have any allergies to medication. The brief procedure may last 15-45 minutes, followed by a recovery period.
Step 1: prepare the patient
The patient lies on an x-ray table. Local anesthetic is used to numb the treatment area. The patient experiences minimal discomfort throughout the procedure. The patient remains awake and aware during the procedure to provide feedback to the physician. A low dose sedative, such as Valium or Versed, is usually the only medication given for this procedure.
Step 2: insert the needle
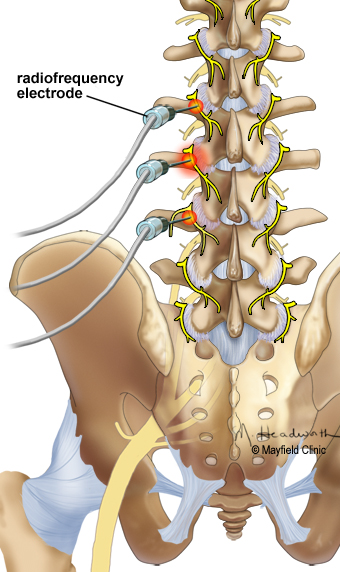
The technique for nerve ablation is similar to that used for diagnostic blocks. With the aid of a fluoroscope (a special x-ray), the doctor directs a thin hollow needle into the region responsible for the pain. Fluoroscopy allows the doctor to watch the needle in real-time on the fluoroscope monitor to make sure that the needle goes to the desired location. Contrast may be injected to confirm correct needle location. Some discomfort occurs, but patients typically feel more pressure than pain.
Step 3: deliver heating current
Once the needle is in place, the patient receives a numbing medication. Then a radiofrequency current is passed through the hollow needle to create a small and precise burn, called a lesion, about the size of a cotton swab tip (Fig 1). The current destroys the portion of the nerve that transmits pain and disrupts the pain-producing signal. The burn takes approximately 90 seconds for each site, and multiple nerves can be burned at the same time.
What happens after treatment?
Most patients can walk around immediately after the procedure. After being monitored for a short time, you can usually leave the office or suite. Someone must drive you home.
Patients may experience pain from the procedure for up to 14 days, but this is generally due to the residual effects of the nerve ablation or muscle spasm. Patients are often up and around and back to work 24 to 72 hours after the procedure. Pain relief is typically experienced within 10 days, although relief may be immediate for some patients and take up to three weeks for others.
Patients should schedule a follow-up appointment with the referring or treating physician after the procedure to document the efficacy and address any concerns the patient may have for future treatments and expectations.
What are the results?
Pain relief may last from 9 months to more than 2 years. It is possible the nerve will regrow through the burned lesion that was created by radiofrequency ablation. If the nerve regrows, it is usually 6-12 months after the procedure. Radiofrequency ablation is 70-80% effective in people who have successful nerve blocks. The procedure can be repeated if needed.
What are the risks?
Radiofrequency nerve ablation is relatively safe procedure with minimal risk of complications. The complications reported in the literature include: temporary increase in nerve pain, neuritis, neuroma, localized numbness, infection, allergic reaction to medications used during the procedure, and/or lack of pain relief (in less than 30% of patients).
mayfieldclinic.com
